Osteoarthritis diagnosis – the stages of OA explained
Osteoarthritis is the most common form of arthritis. The joint most commonly affected, is the knee joint. OA of the knee generally affects people aged 50 and older. However, previous injuries, extreme sports, misalignment of the lower extremities or being overweight may cause osteoarthritis to develop at a younger age.

An osteoarthritis diagnosis (OA) may make you want to find our more about your condition. The joint most commonly affected by osteoarthritis, is the knee joint, but the progression of osteoarthritis is the same for all joints. OA generally affects people aged 50 and older. However, previous injuries, extreme sports, misalignment of the lower extremities or being overweight may cause osteoarthritis to develop in the hips, knees and feet at a younger age.
USE the OMH exclusive code "HEALTH15" to Save 15%Osteoarthritis affects all the main components of the joint, which are:
- the cartilage
- the synovium (also called the synovial membrane)
- the underlying (also called the subchondral) bone
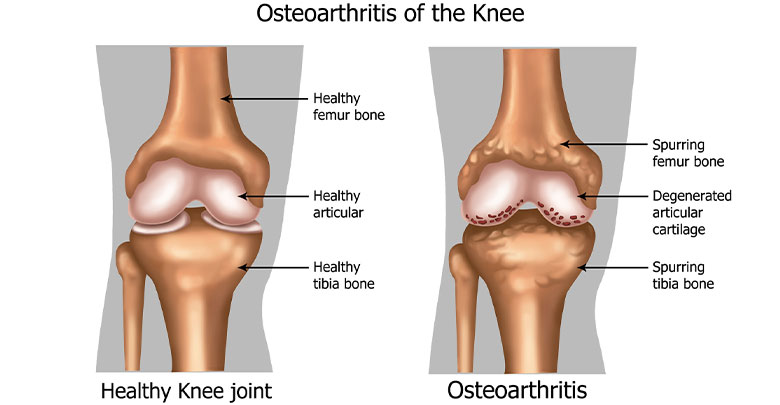
The cartilage is the smooth tissue at the ends of the bones, which allows the bones to slide over each other without any friction and also acts like a cushion between the bones.
The synovium (or synovial membrane) is a soft flexible layer of tissue which lines the inside of the joint – covering every part of the inside of the joint except where there is joint cartilage. The synovium produces a fluid, called synovial fluid, which provides lubrication and supplies vital nutrients and oxygen to the cartilage.
An osteoarthritis diagnosis is made when the cartilage and synovium break down and deteriorate, gradually leading to damage of the underlying (subchondral) bone. This results in pain, stiffness and eventually leads to the loss of normal function since both boney ends of the joint will be rubbing on each other. The process is gradual and happens over a period of years.
Stages 1 – 4 of osteoarthritis diagnosis
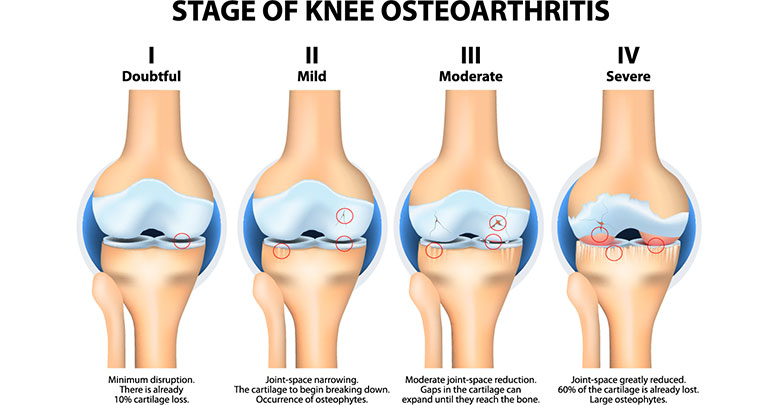
Stage 1 – minor osteoarthritis
At this stage in the development of osteoarthritis the patient may experience some crepitus (crackling or gritty feeling in the joint). There is only slight damage to the cartilage. The patient may have no pain or discomfort, and the joint will look normal on an X-ray.
Stage 2 – mild osteoarthritis
Osteoarthritis moves into stage 2 when the patient starts to notice symptoms of pain and stiffness. On X-ray, there will be evidence of “wear and tear” damage and small osteophytes will be visible. At this point the cartilage will be thinning, but the space between the bones will be normal. In stage 2 there is not yet bone rubbing on bone, and the synovial fluid is not yet affected.
Stage 3 – moderate osteoarthritis
In stage 3 there is an increase in cartilage damage and the gap between the two boney ends will show signs of narrowing. X-rays will show significant cartilage loss. Normal activities such as walking, running, climbing stairs, moving and bending the joint become painful and the joint feels stiff. There will also be early signs of joint inflammation, which will make the joint feel warm and swollen.
The warmth, tenderness and swelling is due to the progression of the arthritis process, and is called synovitis. (Synovitis means inflammation of the synovium.) The synovium becomes inflamed and produces more synovial fluid causing swelling.
Stage 4 – severe osteoarthritis
As the osteoarthritis progresses, the signs and symptoms become more apparent. The space between the bones continue to narrow and the cartilage degeneration is advanced. At this stage almost no cartilage tissue is visible on X-ray. There will be an increase in stiffness, and the inflammation becomes chronic. As a result of the deterioration of the cartilage and synovium, and lack of normal joint lubrication, the patient will have more bone on bone friction.
Depending on the joints affected, normal everyday activities like walking, climbing stairs or going to the bathroom become very challenging. If the hands or fingers are affected, tasks such as opening jars or bottles, doing up buttons, crafting or tasks become difficult. If the spine is affected, many functional daily activities like rolling or getting out of bed, moving from sitting to standing, getting in and out of a car and many other movements become painful and arduous.
What to do if you have a diagnosis of osteoarthritis?
If you have knee or hip osteoarthritis, check out our knee exercise video and our hip exercise video here. These exercises will help you to perform approved optimal physical therapy exercises in order to strengthen the muscles around the joint, and thereby slow down the progression of your osteoarthritis.
As you can see, the gradual progression of osteoarthritis can lead to pain, stiffness and eventually to severe limitations of your everyday activities. However an osteoarthritis diagnosis need not be a life sentence of pain and deterioration.
You may also like to sign up for our free 14 Day Anti-Inflammatory Meal Plan which will help to control the inflammation associated with osteoarthritis. OhMy.Health wants to help you and to educate you about how to protect your joints and prevent the progression of osteoarthritis – enabling you to live your best, happiest and most active life.
References
1. Jordan JM 2008 https://jamanetwork.com/journals/jama/article-abstract/181740
2. Sinusas K 2012 https://www.aafp.org/afp/2012/0101/p49.html
3. Heidari B 2011 (Part I) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3766936/
4. Heidari B 2011 (Part II) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3770501/
5. Pearle A 2005 https://www.sportsmed.theclinics.com/article/S0278-5919(04)00094-8/abstract
6. Phan CM et al. 2006 https://link.springer.com/article/10.1007/s00330-005-0004-5
7. Felson DT et al 2004 https://onlinelibrary.wiley.com/doi/full/10.1002/art.20726